Clinical Laboratories are Turning to Scanning and Printing Solutions to Expand Diagnostic Testing Capabilities as COVID-19 Demands Surge
It is hard to recall another time in this generation when diagnostic testing has been demanded at the same scale or speed as it has been in 2020. Though we’ve experienced widespread outbreaks of many infectious diseases and even contended with other pandemics, no other contagion has had such a dramatic and equal impact on the global population and healthcare system as COVID-19.
As we work to contain the further spread of this virus, a significant emphasis is being placed on increasing testing capacity. Drive-thru and walk-up testing sites are popping up in parking lots and retail stores, and manufacturers are ramping up production of testing kits to help ensure anyone who needs or wants a test can get one. Yet, increasing specimen collection capacity is only going to be fruitful in our fight against COVID-19 if we have the means to quickly process those tests and communicate positive test results back to patients, healthcare providers and contact tracers.
(The faster we can notify others in the community of known/potential exposure and get them into isolation, the more effective we become at mitigating asymptomatic or pre-symptomatic spread. Of course, confirming a positive case also helps to inform treatment plans for symptomatic patients, especially those hospitalized.)
Therefore, the healthcare community must find a way to increase laboratory capacity STAT.
What Clinical Laboratories are Learning from Hospitals as They Both Work to Manage Surge Capacity
Like the rest of the healthcare community, those managing and staffing diagnostic centers have learned a lot from COVID-19 these past several months, particularly the importance of collaboration, communication and (more broadly) widespread technology utilization.
Surge capacity, whether demanded in a clinical or laboratory setting, is only attainable if you are able to somehow increase workflow efficiency, workforce productivity levels and resource availability. In modern healthcare environments, particularly in the middle of a pandemic, that means that process automation is a fundamental criterion.
Patient intake teams have to verify patient identities and capture medical histories quickly to initiate the triage process. Clinicians have to be able to retrieve or update patient records in real time at the point of care to initiate expedite medication or treatment administration. And those charged with collecting, transporting and testing suspected COVID-19 specimen samples must be able to move faster than usual without making any mistakes.
It is critical to instill public confidence in test result accuracy right now. And, though I can’t speak for the reliability of various testing techniques, I do know that care must be given to mitigate the risk of any errors occurring during specimen collection and laboratory processing /reporting. The last thing that anyone wants to do is accidentally compromise the integrity of collected samples.
That’s why it’s imperative that data capture and distribution processes are fully automated from the point of specimen collection to the point of specimen processing (i.e. the laboratory) and then also at the point of care (either a permanent hospital, field hospital or clinic).
Any sort of manual data capture or distribution tasks – even something as simple as completing a pre-test screening checklist at a walk-up testing facility – can lead to specimen mislabeling, processing delays and incomplete or inaccurate patient records. Sometimes, the consequences of these front-line missteps can be quite far reaching. Missing or incorrect label info can render samples untestable and patient misidentification specifically can lead to reporting delays, inaccurate diagnoses and adverse treatment events.
Many hospitals and testing sites already understand this and have taken fast action to equip staff with clinical smartphones, mobile printers, scanners and specialized label solutions designed for use with COVID-19 testing materials to help reduce the risk of these errors and subsequent adverse events.
However, clinical labs need to collectively increase their adoption of these technologies, and they need to do it fast!
When samples come in, lab technicians must be able to scan the barcoded labels on specimen vials to instantly retrieve patient electronic health records (EHR) and verify that the EHR information accurately associates with what’s on the label before starting any testing. Once results are available, they must then be able to scan the vial once again to retrieve and update the correct patient record and prompt a notification to the patient and/or care team. Since specimen samples could be transferred to new vials at some point in the testing process, lab technicians also need the ability to print and affix new labels on the spot.
As the U.S.-based Innovative Genomics Institute (IGI) learned during its conversion to a COVID-19 testing facility, it’s not easy to create an accurate, efficient and safe lab environment capable of managing high throughput without the right print-scan solutions integrated into every aspect of the diagnostic testing process.
Like Hospitals, Testing Labs Must Fast Track Technology Implementations to Increase Capacity. But, Like Hospitals, They Can’t Afford to Compromise Solution (or Worker) Performance for the Sake of Speed.
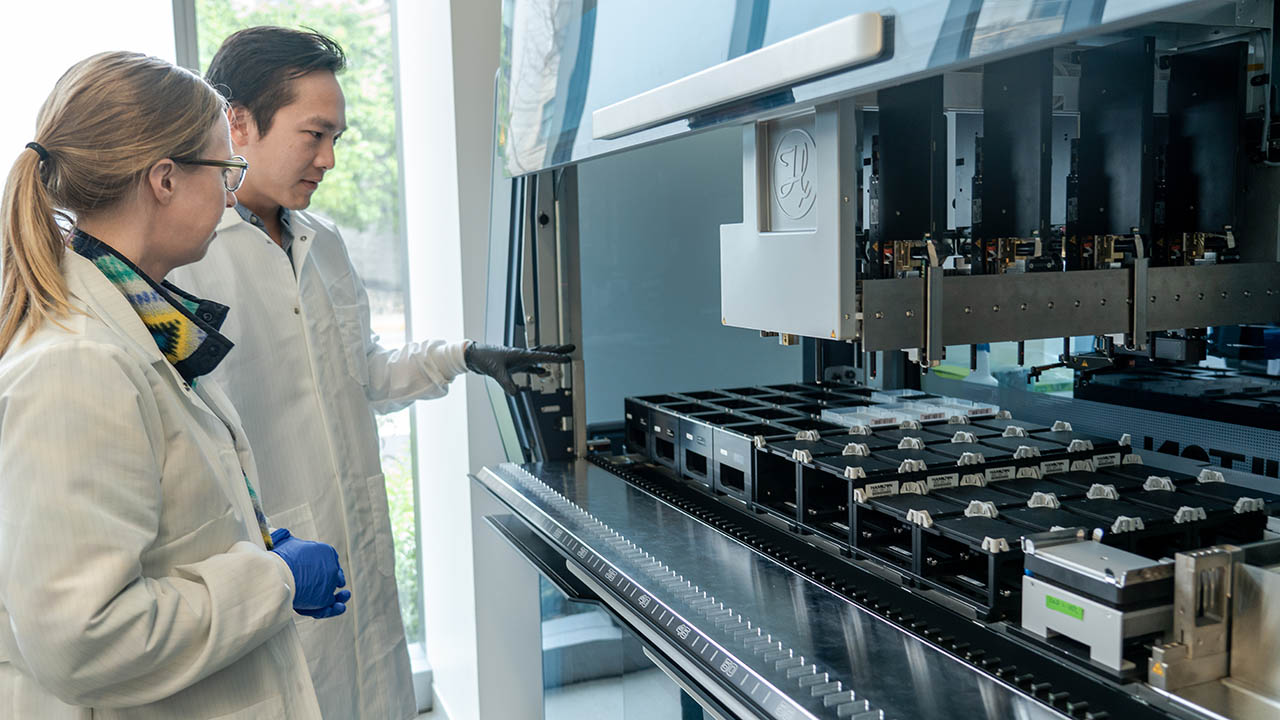
Established in 2014 as a partnership between the University of California, Berkeley and the University of California, San Francisco, IGI normally operates as a genome editing research institute. But when the stay-at-home order was declared due to COVID-19, the IGI team decided it didn’t just want to walk away from its research: it wanted to help. The fastest way to make an immediate impact on the local community was to launch a COVID-19 testing lab because testing was scarce and the techniques were familiar to the researchers.
Once fully up and running, the team wanted to be able to process up to 1,000 specimens per day and deliver results to patients in less than 24 hours, which many agreed was an ambitious but achievable goal with the right equipment and technology tools available to maximize output.
Therein lay the challenge, at least in the beginning.
As a first-time testing facility, IGI didn’t fully appreciate the clinical lab technicians’ core dependency on technology for positive patient identification, proper specimen handling, quality control and reporting. And it took a lot of trial and error to realize that not all barcode scanners are suitable for healthcare applications and not all printers and labels are optimized to work together in the way needed for compliant specimen labeling.
But once lab managers understood how significantly device performance impacts staff output, IGI reached out to Zebra for technology solutions that were purpose-built for healthcare and proven in numerous different clinical settings, including hospitals, testing sites and diagnostic labs.
IGI implemented barcode scanners that enabled technicians to read labels through plastic bags, which instantly reduced the number of times test kits had to be opened and closed, and selected barcode labels that would maintain readability after being wiped with disinfectants – both of which offered significant efficiency gains. The IGI team also worked with Zebra to select the right hardware + software + media for all applications and optimize various component integrations in order to increase the performance and reliability of the scan-print solution.
Migrating to a purpose-built and proven healthcare-grade technology solution also helped to increase lab safety. For example, the use of Zebra barcode scanners eliminated the need for technicians to touch samples and risk direct contact with potential contagions and allowed for repeated (yet, easy) device wipe downs with chemical-based disinfectants per the guidelines recommended in this video:
IGI also gained several other benefits once it implemented the right scan-print solution, as you can read about in this case study:
The Innovative Genomics Institute Pivots to Combat the COVID-19 Pandemic
I think it’s important to note, though, that IGI’s success in specimen testing did not come from simply automating certain data capture actions or integrating barcode scanners and label printers into its workflows. It resulted from IGI’s willingness to invest the effort into finding the right technology solutions, even if it took a little bit of time to figure out what those were, and an unwillingness to settle for rudimentary off-the-shelf scanners or printers for the sake of buying speed.
In fact, if you take anything away from IGI’s experience, it should be that:
- COVID-19 testing labs need reliable scanning and label printing solutions to help mitigate mistakes and delays and increase confidence in the reliability of test results.
- Healthcare-grade solutions are as fast and easy to deploy as off-the-shelf devices. In fact, they may be even faster to deploy since solution providers already understand interoperability requirements with Laboratory Information Management Systems and know-how to configure each solution components to facilitate that highly automated and efficient end-to-end workflow.
- Not all technology devices are safe to use in highly controlled clinical laboratory environments. Every healthcare facility has strict infection control protocols, particularly when it comes to the cleaning of mobile and desktop devices that are constantly touched by those who work in close proximity to patients. However, diagnostic testing facilities have the added responsibility of preventing cross-contamination with specimen samples. Unless the scanners, printers and even labels used in your lab can be properly disinfected at frequent intervals, and without the risk of damage, then they could potentially pose a safety risk to your staff.
Remember, labs tapped for COVID-19 testing are having to create a much more controlled environment than other clinical diagnostics may demand. Samples must be handled more carefully, tests must be conducted at much faster rates and reporting must happen immediately, especially when positive cases are confirmed.
Take the time to understand which technology solutions will facilitate an effective diagnostic workflow in your lab and allow for a constant communication flow between your technicians and the people eagerly awaiting their call/email. Doing so will help eliminate testing and reporting delays even as demand surges and, in turn, increases the ability of the healthcare community to treat positive cases, conduct effective contact tracing and curb infectious disease.
###
Editor’s Note:
Want to learn more about how Zebra worked with IGI to automate its new specimen testing lab in just one week? Or how we can help you increase your lab’s workflow efficiency and testing capacity? Contact our Healthcare team here.

Rikki Jennings, BSN, RN, CPN
Rikki Jennings, BSN, RN, CPN is currently the Chief Nursing Informatics Officer (CNIO) at Zebra Technologies where she is responsible for combining her knowledge of patient care, informatics concepts, and change management to effectively address the information and knowledge needs of healthcare professionals and patients to promote safe, effective, and efficient use of IT in clinical settings. She also serves as the strategic liaison for health IT efforts representing nursing and clinician needs.
Early in her nursing career, Rikki recognized a disconnect between purchased technologies and the understanding of their intended value at the bedside by her fellow clinicians and pursued Nursing Informatics. She is passionate about the utilization of technology to support safer, more effective care models. Over the past several years, her work in the healthcare IT industry has provided her an in-depth knowledge of the workflows and utilization of clinical technologies including clinical communication systems, bedside technology solutions, and data analytics tools in hospitals across the country. In 2019, Rikki was recognized in Crain’s Chicago Business’ Notable Women in Healthcare list.
Rikki holds a Bachelor of Science in Nursing from University of Iowa.






